What does a new floater mean? Should you be worried? What is a vitreous detachment? How can you tell if I have a retinal detachment?
If you have had retinal detachment surgery, what will your vision be afterward? (Not necessarily what the doctors say.
After retina surgery, my returning vision was not what I expected. I feared I had another detachment, and had two additional days of remaining facedown until I could see a doctor. When it turned out to be a normal progression, I created these images to provide reassurance to other patients who may be concerned about their vision after detached retina repair. (My online search for such reassurance yielded only images of eyeballs. )
If you have recently had surgery and are looking for reassurance about your vision, please scroll right down to “Vision after retinal detachment repair.” You can read the rest later.
If you think you may have a detached retina, call and make an appointment with an ophthalmologist (preferably a retina specialist) immediately, then read on.

My story: I had been very nearsighted since childhood and had floaters, so I had been warned the be aware of retinal detachment symptoms.
I had cataract surgery six months prior to my first detachment. Cataract surgery increases risk of retinal detachment—one percent of cataract surgery patients will experience a detachment. (I repeat, it’s a one percent risk. My improved vision after cataract surgery was worth that risk, even though I was unlucky twice, as you will discover below. After my cataract surgery, I had the best vision of my life.)
Retinal detachment surgery increases the risk of developing cataracts if you haven’t previously had cataract surgery. If you have recovered from retinal detachment and your vision gets worse, you probably have developed cataracts. Cataract surgery is much easier for a patient than retinal detachment surgery, so you have already made it through the hard part.
The descriptions and illustrations below are based on my own experience and meant to help others. Also, please note, I’m not a doctor. The percentages I cite are the best I can ascertain from the research I have read. (Apparently few doctors have had both detached retinas and have PhotoShop skill, so I’m volunteering.)

Posterior vitreous detachment (PVD)
I had the sudden appearance of a wiggly gray floater in my left eye, like a hair was in front of my eye that I couldn’t brush away, and flashes of light in my peripheral vision. (It was like a lightening storm occurring far to my left, but the flashes remained to the far left when I turned my head. The flashes continued when I shut my eyes.)
I went to a retina specialist the next morning. I had a posterior vitreous detachment (PVD), which is not uncommon as eyes age.
Close examination (this includes applying uncomfortable pressure) revealed no tear. A PVD has about a 10–15% chance of causing a retinal tear; a symptomatic PVD is more likely to cause a tear. A retinal tear leads to a retinal detachment if fluid flows through the hole created by the tear and collects behind the retina. A retina tear has a 30–50% chance of causing a detachment. (Those risks combined means that a PVD has only about a 3–8% chance of leading to a detached retina.)
Retinal detachment in my left eye
Two weeks later, I thought the floater had settled into a gray area at the top left of my vision (see image).
I went back to the retina doctor because I now had a large gray floater in my right eye that I thought was a new PVD. I was correct in that my right eye had a typical vitreous detachment. Fortunately, the doctor examined both eyes. The gray area was the result of a retinal detachment in my left eye.
I had asked what to watch for to know if I had a detachment. I was told it would look like a dark curtain was coming down, or I might see a shower of black spots. I had neither of those symptoms, but others have told me they did experience what was like a curtain moving down into their field of vision.
As you may recall from elementary school, the curve of the cornea creates an upside-down image on the retina. When I saw a gray spot in the top of my vision, it was because fluid had seeped behind my retina at the bottom right.
I had emergency surgery a few hours later (eight hours after I last ate).

Retinal detachment surgery
Retina surgery is not particularly painful. The retina itself does not have pain sensors, and the flashes of light that may accompany a vitreous detachment are a sign from your body, as the retina can not send pain signals as a warning.
Feel free to skip the rest of this section if you are squeamish. (I had been too squeamish to considered surgery to correct nearsightedness. Now, after six+ eye surgeries, I’m pretty tough.)
There are several different types of procedures that may be used to repair your detachment:
A simple retinal tear may be repaired with a laser to secure the retina to the eye wall around the tear. This can be done in an ophthalmologist’s office. (Great outcome if this works for you. The only discomfort is the contraption that holds your eye open during the laser treatment. Be grateful.)
A detached retina may be repaired with pneumatic retinopexy. A laser is used, as above, then a gas bubble is inserted to push against the retina and hold it to the eye wall so that scar tissue can form and hold the retina down. (This is a simpler version of vitrectomy surgery, below.)
A scleral buckle (a thin flexible band) may be surgically placed around the outside of the eyeball to hold the retina in place. This can be done as a stand-alone procedure, or with a vitrectomy. (The scleral buckle will elongate the eyeball, so the eye will become more nearsighted.)
During a vitrectomy, the vitreous gel in the eye is removed, and replaced with either a gas bubble or an oil bubble to apply pressure and hold the retina in place as it heals. Often, head positioning is important after surgery. The bubble needs to press against the area of the tear, so remaining facedown, or lying on one side, is often required for several days.
A gas bubble will dissipate on its own over several weeks as it is replaced with fluid, just as the fluid in the eye is naturally replaced with fresh fluid over time. (The images and text below show what this looks like to the patient.)
An oil bubble provides a stronger tamponade and, unlike a gas bubble, the patient does not have to avoid high altitudes or air travel. The oil bubble is also strong enough that strict head positioning may be unnecessary. However, unlike a gas bubble, the oil will not dissipate. For best vision, the oil will need to be removed with another surgery. While the oil is in the eye, vision is distorted so that, for example, a nearsighted eye needs a correction typical for a farsighted eye.
General anesthesia is not typically used for retina surgery. I was given medication so that I was unaware and didn’t feel pain for the initial injections and cutting. After a few minutes I was semi-alert and knew what was happening. I could ask for more medication when I felt pain. (While, as I reassured you above, the retina does not have pain sensors, the other parts of the eye can experience discomfort, or more than discomfort, a.k.a. pain, without medication.)
My left eye experience was not typical, complicated by the fact that I was moving from Minnesota to Ohio a few weeks after the surgery. My surgeon, with my agreement, opted for a “belt plus suspenders” approach for highest probability of success.
I had emergency vitrectomy surgery, replacing the vitreous with a gas bubble, and laser repair, plus a scleral buckle. This increased the success rate (successful repair without another surgery) to 94–96%.
When I returned for my post-op visit, the surgeon could see that the repair wasn’t holding—I had more fluid behind my retina. He suggested immediate surgery to replace the gas bubble with an oil bubble. I knew this would mean two more surgeries, so I opted to spend a few more days of facedown discomfort to try and avoid more surgeries. I had laser surgery (in the office, see above) to build a barrier around the leak, and remained facedown for several more days. My Monday morning appointment showed that the repair still wasn’t holding. I had a second vitrectomy to replace the gas with a silicone oil bubble. I would need a third surgery, months later, to replace the oil bubble with saline.*

Retinal detachment in my right eye
A year after the left eye detachment, I saw a vague spot of shadow in my right eye as I walked down stairs. I thought I was imagining it, but it happened a couple of times. Knowing I was increased risk for a second detachment (a 4% risk—much higher than normal, but still low), I was worried. I made an appointment with a retina specialist. The spot was so infrequent and vague that it was more of a premonition over a few days rather than an actual spot in my vision. It was precisely a year after the first surgeries, was I imagining the vague shadow?
Retina specialists encourage patients to be seen immediately with any new floater, no matter how vague.
I saw a specialist on Friday. I did have a detachment in my “good eye.” On Sunday morning, I had another vitrectomy, with a laser to seal around the tears, and a gas bubble to hold the retina in place while scar tissue formed to hold the retina.
For me, because of the location of the tears, remaining facedown for a week was worse than surgery. (I did finally have time to listen to an unabridged recording of War and Peace.) There are also lots of eye drops to fill your days; I recommend you make a checklist.
Vision after retinal detachment repair with a gas bubble
One week post-surgery: Panic
I had read and been told that, as the gas bubble was replaced by fluid, my vision would return from the top, as if I was coming up from underwater. That became true after about three weeks, but at one week post-surgery my vision was frighteningly similar to a large, new retinal detachment. The top of my vision was dark and worse than the bottom.
Due to my previous experience, I feared the repair was not holding. When I called the emergency number, the doctor on call agreed that what I saw might be another detachment, or it might just be fluid returning. Remaining face down would keep a detachment from damaging my vision, so I had an two extra days of that.
When I saw the doctor, I could not see a hand in front of my face (“How many fingers?” only ESP could provide a clue). The doctor said everything looked perfect, and seemed surprised at my concern. (Note: My macula was not affected. For patients who have a detachment that involves the macula, vision is more severely affected before surgery, so vision is often better after surgery than it was prior.)

Two weeks post-surgery: A sliver of clear vision
Over the next week, there was a “horizon line” between the gas and the fluid, and the top became less dark. Overall vision was poor. However, if I held my hand within a few inches from my eye and looked straight down, I could see my fingers clearly (a hopeful sign?). After about two weeks, a saw a flash of clear vision in a sliver right above the horizon line, and a brightness in that area.
Three weeks post-surgery: Vision begins to return
After three weeks—and timing varies depending on the type of gas—the bubble was small enough that I could see over it. The top of my vision returned to it preoperative state!
The bottom did look like I was looking through a swimming pool. By the next week, wearing my glasses, and looking through just the top, I could read the 20/20 line on the eye chart! (It may take six months to achieve best acuity.)
The doctor said that since my macula was not involved (I caught the detachment early) this outcome was not unexpected, but I was not told it was even possible.


Curbs can be dangerous
Looking straight down, through the gas bubble, offered clearer vision than looking straight ahead, but what I saw was enlarged and distorted. This caused double vision with both eyes open, and—caution— curbs are not where they appear.
Reflections
As the bubble continued shrinking, I noticed rays of reflected light coming from the bubble. (I wasn’t able to draw this very well, as I did it from memory after recovery, but you should be able to get the general idea of it.) My vision was normal over the bubble in low consistent light, but looking at a screen, for example, included lots of reflections. In some situations, an arch of light appeared like a yellow rainbow.


The bubble may break apart and reform
Around this time, I had an abrupt hard fall. For a few hours I had multiple bubbles, which were actually interesting to observe. They reformed into one.
As the bubble shrank and I could keep a close eye on it (little joke), I had a mini movie inside my eye. In certain lights the bubble was colorful, and actually pretty.
A bouncing ball
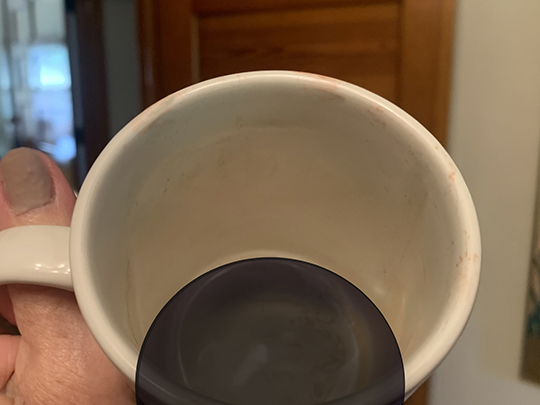
At seven weeks, the bubble was just small enough that I could see it bounce a bit side to side as I walked up stairs. The bubble became the right size that an empty cup looked like there was coffee left. I could laugh a bit as I eagerly awaited its disappearance. I could tell it was shrinking a bit every day.

Eight-and-a-half weeks post-surgery
Every morning I would wake up and look to see if the sing-a-long size bouncing ball of a gas bubble was still there. After eight-and-a-half weeks, it was gone. I was permitted to fly on an airplane again (albeit too late for our canceled vacation).
The sight in my right eye returned to my pre-detachment vision!
To fellow patients: I wish you much success, as well.
*My left eye improvement, perhaps because the tear and the detachment were both larger, has been less successful.
The vision in my left eye slowly improved after the oil bubble was removed, and I am now very grateful that I have good vision with glasses. Before the detachment, a lens implant during cataract surgery had given me 20/20 vision in that eye. The scleral buckle now causes nearsightedness. My uncorrected vision is now about 20/100 in my left eye, but with glasses I am very pleased that, on a good day, it is almost 20/30. With the oil bubble, the best correction was 20/40 for distance, but reading was difficult. I do have a small leftover oil bubble (sometimes one little bubble, other time many smaller bubbles) and some pigment in the vitreous from the multiple surgeries, as well as very poor vision first thing in the morning, but overall, I feel very fortunate. I have stacks of book around my house, unread due to lack of time rather than poor vision. On clear days, I often pause to marvel that I am able to see individual leaves on trees. I will never take my vision for granted.